Why Medicaid Redeterminations Are Paused in 12 States
Medicaid disenrollment issues prompt CMS to pause state redeterminations
The Centers for Medicaid and Medicare Services (CMS) is calling on a number of states to pause Medicaid redeterminations after identifying a number of disenrollment issues and procedural errors.
In a letter published by CMS last week, the agency ordered states to temporarily halt determinations until their concerns and violations - some of which are highlighted below - are addressed:
Of the 5.5 million people who have lost coverage due to Medicaid redeterminations since April 2023, about ¾ lost coverage due to procedural disenrollment. This means that a high volume of Medicaid beneficiaries have lost their coverage not because they are no longer eligible, but because they did not complete the necessary paperwork or meet administrative requirements in time.
Some beneficiaries have been disenrolled due to system errors. For example, states are required to auto-renew individuals if the state can verify their income information. However, CMS has found that some states’ system glitches have prevented electronic data matching, meaning that income can’t be verified and individuals have lost coverage despite their eligibility.
CMS also found that many disenrollments were being conducted at the household level, despite the fact that states are required by federal law to conduct reviews at the individual level. For example, if someone is no longer eligible for Medicaid, it should not impact the coverage of someone else in their family. However, CMS found instances in which entire households lost coverage even if just one individual in the household was no longer deemed eligible for Medicaid, Medicare or CHIP.
These disenrollments can be unintentional but have a serious impact on those who rely on Medicaid for essential health services. This issue brings into focus the ongoing challenges related to Medicaid, health insurance, and the complexities of maintaining continuous coverage for vulnerable populations.
What are Medicaid redeterminations?
Medicaid redeterminations are mandatory reviews conducted by state Medicaid agencies. This annual or semi-annual review aims to assess whether current Medicaid beneficiaries still meet the program's eligibility criteria. During this process, recipients need to provide updated income statements, proof of residency, and other information to confirm that they still qualify for benefits.
When the COVID-19 Public Health Emergency (PHE) was declared in 2020, the federal government began to provide additional Medicaid funding to states in exchange for states adopting a provision known as Continuous Enrollment. This provision meant that states could not conduct Medicaid eligibility reviews and disenroll people from the program, and was put in place to ensure that no one would lose health insurance during a time when medical care was needed so critically by so many.
However, states were able to resume Medicaid eligibility reviews (a process known as redetermination) starting in April of 2023, and the process of “unwinding” continuous enrollment and recommencing Medicaid redeterminations has proven to be complex and fraught with challenges.
Why the pause?
The redeterminations process, although essential, has run into a number of operational and systemic hurdles. The pause in some states allows time for CMS and state agencies to review and adjust the redetermination procedures, ensuring that beneficiaries are not unduly removed from the program. Given the critical importance of Medicaid in providing healthcare to low-income individuals and families, it’s imperative to minimize procedural disenrollments to the greatest extent possible.
Implications for beneficiaries
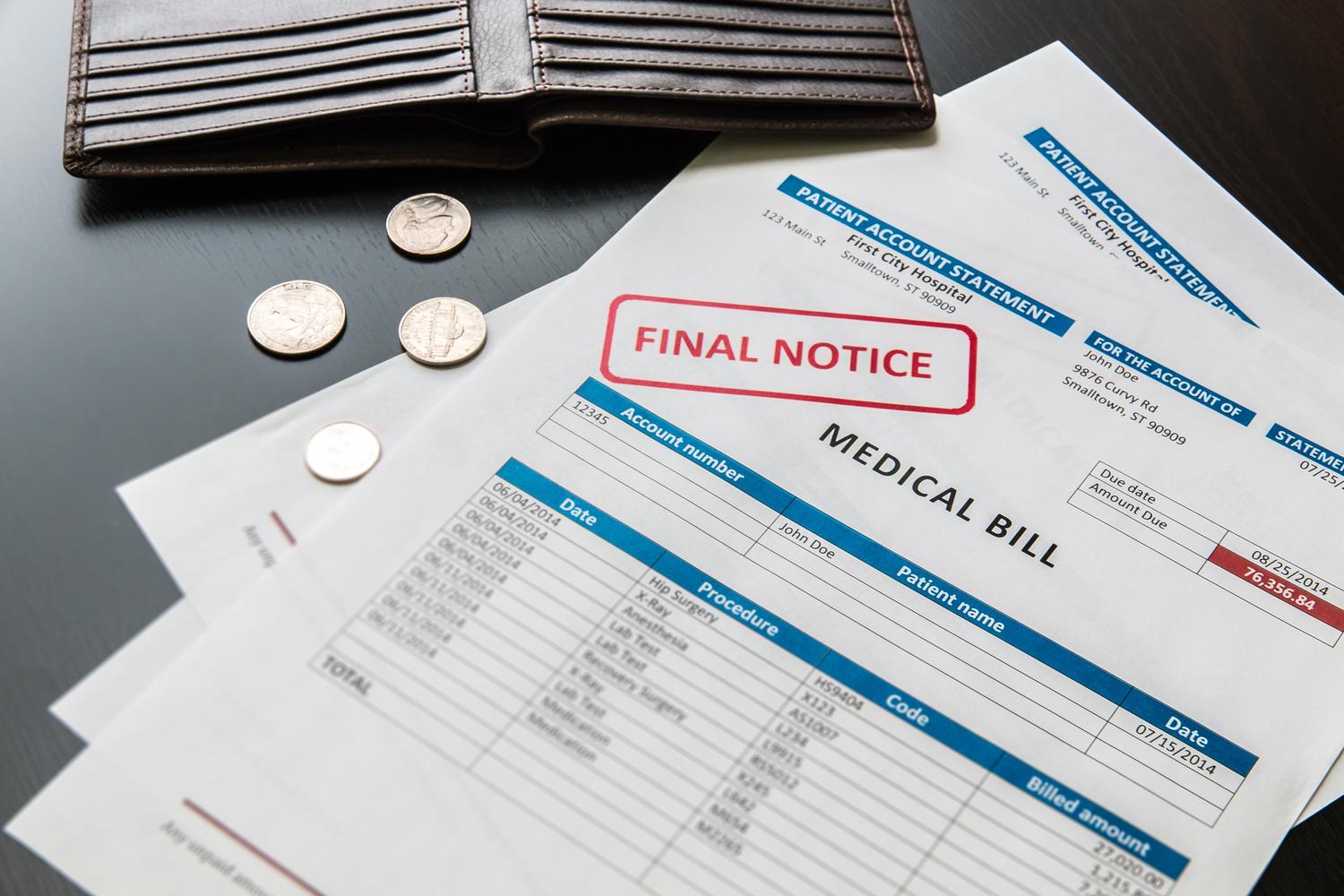
The disruption caused by procedural disenrollments can be significant, affecting not just individual health but also public health metrics. Losing Medicaid coverage often means losing access to preventive care, which in turn can lead to worsened health conditions and higher healthcare costs down the road. Disenrollments can also disrupt the continuity of care for chronic conditions, mental health services and other long-term health needs.
What’s being done to address the issue?
CMS is actively working with states to find solutions to reduce the number of procedural disenrollments. These solutions include simplifying administrative procedures, providing clearer instructions to beneficiaries, and using automated systems to remind beneficiaries of pending redeterminations.The objective is to make the redetermination process as seamless as possible while ensuring that only those who genuinely meet the eligibility criteria continue to benefit from the program.
CMS is also requesting that the 12 states (who have not been specifically named) pause redeterminations, reinstate coverage for individuals whose coverage was inappropriately terminated, and implement mitigation strategies to prevent future inappropriate disenrollments.
A health care solution for all
The complexities surrounding Medicaid redeterminations and procedural disenrollments highlight the fragility and intricacies of healthcare access in the United States. As policy measures evolve and legal battles continue, platforms like Sesame offer a reliable, convenient option for healthcare services.
Sesame provides an array of healthcare services that can be accessed at affordable prices, regardless of a patient’s insurance status. From telehealth consultations to in-person doctor visits, the platform is designed to provide fast, high-quality care for all. If you or a loved one has been disenrolled from Medicaid or are concerned about the redetermination process, Sesame offers a pathway to continue accessing the healthcare services you need, when you need them.